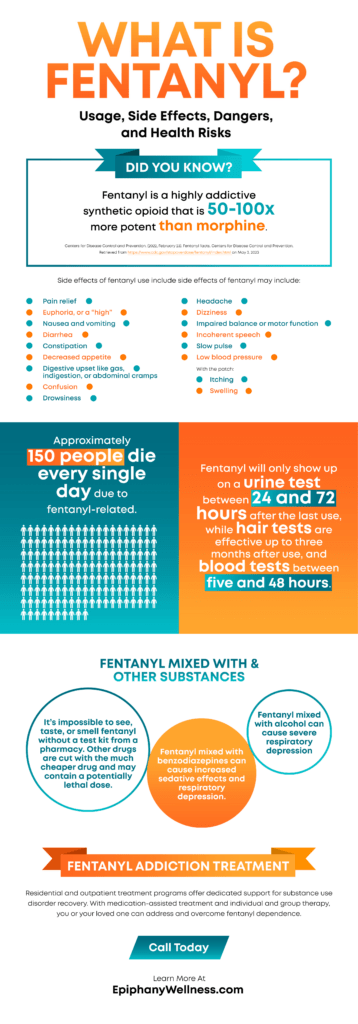
What Is Fentanyl? Usage, Side Effects, Dangers, and Health Risks (Infographic)

Fentanyl is a synthetic opioid that’s used in clinical settings to treat pain. It’s similar to morphine but much more potent. It’s also illicitly produced and mixed into other drugs, such as cocaine and heroin, leading to unintentional use with tragic results.
Fentanyl overdose has been a leading and highly publicized cause of death for Americans. From 2019 to 2020, there was a spike in fatal overdoses involving synthetic opioids, including fentanyl.[1]
Drugs laced with fentanyl have become ubiquitous in the US, raising the risk of overdose for everyone involved in illicit drug use. Here’s what you need to know about fentanyl, its risks, and how to seek help for yourself or a loved one.
What is Fentanyl?
Share this image on your website
Fentanyl is a synthetic opioid. An opioid is a type of drug that interacts with the opioid receptors in the body and brain to reduce the perception of pain. Synthetic opioids like fentanyl are synthesized in a lab to mimic the effects of natural opiates, but it can be up to 100 times stronger.
Fentanyl was originally developed as an analgesic – or painkiller – for surgical use. Like other opioids, it was intended to treat pain conditions such as post-surgical pain, pain with cancer treatment, and pain associated with end-of-life. When it’s used for pain, it’s under the careful supervision of a physician.
Pharmaceutical fentanyl comes in many forms, including transdermal patches, lozenges, lollipops, and intravenous injections. Along with prescribed uses, pharmaceutical fentanyl may be used illicitly by extracting it from a patch and injecting it.
Illicitly Manufactured Fentanyl
While legal fentanyl can result in overdoses, illicitly manufactured fentanyl (IMF) is largely responsible for the recent cases of fentanyl-related overdoses. It’s made its way into the illegal drug market because it can enhance the experience of other drugs, such as heroin.
Manufacturers often lace drugs with fentanyl because of its potency, which makes the resulting combination more addictive, more potent, and cheaper, though it also makes them more dangerous.
IMF comes in powder and liquid forms. The powdered version looks like other powdered drugs, including methamphetamine, heroin, and cocaine. It can be mixed into these drugs easily or made into pills that look like other prescription opioids.
The biggest danger with fentanyl, besides its potency, is that people don’t realize their drugs are laced with it. IMF can also be found in nasal sprays, eye drops, or other forms, including counterfeit pills. According to the Drug Enforcement Administration (DEA), there are many street names for fentanyl, including Jackpot, Apache, Friend, Dance Fever, Tango & Cash, and Murder 8.[2]
Effects of Fentanyl
Though fentanyl may be prescribed in certain situations, it’s never completely safe. Like all drugs, fentanyl carries risks with its use. If it’s been prescribed, your physician determined that the benefits outweighed the risks.
The effects of fentanyl can vary from person to person based on factors like:[3]
- The individual’s size, weight, and sex
- Other drugs that are in the system at the time
- The amount of fentanyl consumed
- The strength of the drug and its form
- The individual’s usual fentanyl use
The side effects of fentanyl may include:
- Pain relief
- Euphoria, or a “high”
- Nausea and vomiting
- Diarrhea
- Constipation
- Decreased appetite
- Digestive upset like gas, indigestion, or abdominal cramps
- Confusion
- Drowsiness
- Headache
- Dizziness
- Impaired balance or motor function
- Incoherent speech
- Slow pulse
- Low blood pressure
- With the patch, itching or swelling at the patch site
With regular use, fentanyl may cause:
- Reduced libido
- Chronic constipation
- Menstrual problems
- Respiratory impairment
- Mood instability
When used intravenously, fentanyl may lead to an increased risk of vein damage, contracting tetanus or another infection, or contracting bloodborne illnesses like HIV, hepatitis B, or hepatitis C.
Fentanyl and Other Drugs
The risks and effects of fentanyl increase when it’s mixed with other drugs, including prescription medications, over-the-counter medications, or substances like alcohol.[4]
- Fentanyl mixed with monoamine oxidase inhibitors (MAOI) antidepressants can cause severe mood instability.
- Fentanyl mixed with benzodiazepines can cause increased sedative effects and severe respiratory depression.
- Fentanyl mixed with alcohol can cause increased sedative effects and severe respiratory depression
Fentanyl Withdrawal
Fentanyl and its injectable form Sublimaze, are extremely powerful substances. Stopping use on your own can be difficult and hazardous without assistance. The fentanyl withdrawal symptoms typically begin within 12 hours of the last dose and can last from a few days to a week. After stopping use, the first few days are typically the worst.
The symptoms of withdrawal may include:
- Alternating between body chills and flushing
- Insomnia
- Irritability
- Watery eyes and nasal congestion
- Vomiting and nausea
- Loss of appetite
- Increased blood pressure and heart rate
- Body aches
- General weakness
- Depression and anxiety
- Extreme cravings
Fentanyl and Overdose
Fentanyl and other synthetic opioids are commonly involved in overdose deaths. Over 150 people die each day from overdoses involving synthetic opioids like fentanyl.[5] Fentanyl can be deadly even in small doses.
It’s impossible to see, taste, or smell fentanyl, so other drugs may contain potentially fatal levels without detection. The only way to know if drugs have been laced with fentanyl is with a fentanyl test kit, which is widely available at pharmacies.
Testing isn’t perfect, however. It’s important to be cautious and understand the signs of fentanyl overdose:
- Constricted, “pinpoint” pupils
- Slow or weak breathing
- No breathing
- Body limpness
- Cold or clammy skin
- Drowsiness or loss of consciousness
- Skin discoloration, particularly around the lips and nails
- Seizures
Related: What Does A Fentanyl Test Kit Do?
How to Handle an Overdose
Overdose symptoms can be subtle. If you suspect an overdose at all, reacting quickly can be the difference between life and death.
Call 911 immediately.
- Administer naloxone if available.
- Try to keep the person awake.
- Turn the person on their side to avoid aspiration.
- Stay until emergency services arrive.
If you’re concerned about legal ramifications, most states have laws in place to protect both the person experiencing an overdose and the person seeing emergency medical attention. Don’t let the fear of legal trouble prevent you from seeking help.
Overdoses can happen in situations you may not expect. It’s best to be prepared by keeping naloxone on hand. This life-saving medication blocks opioids and can reverse the effects of an overdose. Naloxone is available over the counter at pharmacies in most states.
What Is Rigid Chest Syndrome?
In some cases, synthetic opioids like fentanyl cause a seizure-like reaction with muscle spasms, locked limbs, and a rigid chest. This can prevent a person from breathing properly, so if you witness this, treat it as an overdose and administer naloxone.
How Is Fentanyl Addiction Treated?
Opioids like fentanyl produce feelings of euphoria, which make them highly addictive for many people – despite negative consequences. When this occurs, it’s known as opioid use disorder (OUD). According to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM 5-TR), people with OUD experience some or all of the following patterns within a 12-month period:[6]
- Taking higher amounts of opioids or for a longer period than intended
- Spending a lot of time seeking opioids, using opioids, or recovering from the effects
- Having cravings or a strong desire to use opioids
- Unsuccessful efforts to control or stop using opioids
- Struggling at home, work, or school
- Continuing opioid use despite interpersonal problems
- Giving up once-loved activities to pursue – or because of – opioid use
- Reckless behaviors like driving under the influence of opioids
- Increased tolerance for opioid
- Experiencing opioid withdrawal syndrome
- Taking opioids or related substances to relieve opioid withdrawal symptoms
Fortunately, there are effective treatments for opioid use disorder. Depending on the individual’s needs, OUD may be treated with evidence-based modalities like medications, counseling, and behavioral therapies.
Here are the two medications approved by the Food and Drug Administration (FDA) for opioid use disorder:
Methadone
Methadone is a long-acting opioid agonist that’s effective for treating OUD. It’s a type of medication-assisted treatment. It works by replacing a drug of dependence with a safer, legally prescribed substitute, often in conjunction with other treatment options.
Because methadone is a Schedule II controlled substance, it must be prescribed and administered by medical professionals. They are involved in every stage of the process, from prescription to ongoing use, carefully monitoring progress.
Buprenorphine
Buprenorphine was the first medication used to treat OUD. It’s an opioid partial agonist that activates the opioid receptors in the brain, but to a lesser extent than a full agonist.
When taken as prescribed, buprenorphine is safe and effective for diminishing the withdrawal symptoms and physical dependence on opioids, decreasing the risk of overdose, and reducing the risk of misuse.
Buprenorphine must be prescribed and administered by a medical professional. The dose and length of treatment may be adjusted as needed to produce favorable outcomes. In some cases, buprenorphine is combined with naloxone (suboxone) to prevent accidental or intentional misuse.
Along with medication, OUD treatment encompasses many other aspects of support. The key to successful treatment is an individualized approach that takes the medical history, mental health, and specific challenges into consideration.
What Are the Steps in Fentanyl Addiction Treatment?
There’s no one-size-fits-all approach to fentanyl addiction treatment. Each treatment approach is tailored to the individual’s needs, but may include:
Medically Managed Detoxification (Detox)
Medically managed detoxification, or detox, can be a first step in a treatment plan. Medical professionals monitor an individual as the body rids itself or opioids, and can provide comfort medication to help alleviate physical and psychological withdrawal symptoms.
Inpatient Rehabilitation
Inpatient rehabilitation, or residential rehabilitation, is 24/7 care in a hospital or residential treatment center. In this setting, people with OUD can receive medication-assisted therapy (MAT), individual and group counseling, addiction education, and behavioral therapies as indicated.
Living within a treatment facility on a short-term basis provides unwavering support from clinical staff and other people experiencing similar challenges and struggles. There’s no stress of home, work, or school to cause distractions or promote relapse, so people can focus solely on their recovery and well-being.
Outpatient Rehabilitation
Outpatient rehabilitation may take place within an intensive outpatient program (IOP) or an outpatient program. People attend onsite counseling sessions and behavioral therapies, much like inpatient services, but they’re free to return home in the evening when treatment is completed.
IOP is a higher level of care than outpatient services for people who need more rigorous treatment programs but don’t require full hospitalization. In some cases, IOP may be a step down from hospitalization to programs with more flexibility and independence, such as traditional outpatient or aftercare programs.
Aftercare
Aftercare, also known as sober living or continuing care, is a program that’s designed to help people transition into everyday life after OUD treatment. It provides community support and treatment modalities to prevent relapse, teach stress management and coping skills, and build a strong support system. Attending sober events can serve as a supportive tool in staying dedicated to a sober way of life.
How Long Does Fentanyl Addiction Treatment Last?
Because all OUD treatment programs are tailored to the individual, the length of treatment can vary significantly by the treatment protocols, the severity of the addiction, and the adherence to treatment.
Substance use disorders like OUD are chronic conditions. There’s no finish line for recovery – it takes a lifelong commitment to sobriety. Treatment programs are designed to “step down” from more intensive treatments to more flexible treatments, building strength, coping skills, and healthier habits every step of the way to adopt a healthier lifestyle.
Struggling with Fentanyl or Opioid Use Disorder?
Fentanyl is a powerful, dangerous synthetic opioid that’s used in medical settings but may be found in an array of other street drugs, often leading to fatal overdoses.
If you’re struggling with fentanyl or OUD, you’re not alone. Addiction is not a weakness but a mental health condition that requires treatment to overcome. With the right support and knowledge, you can overcome your addiction and find a healthier path forward. Contact Epiphany Wellness today to see what life could be like without opioids.
Fentanyl Testing FAQs
Still have questions? Find out more about fentanyl, opioid use disorder, and treatment options.